Crohn's disease is a chronic inflammatory bowel disease that can affect any part of the gastrointestinal tract. Symptoms can range from mild to severe and can vary greatly from person to person. This guide will provide a comprehensive overview of Crohn's disease, including its symptoms, causes, and available treatment options.
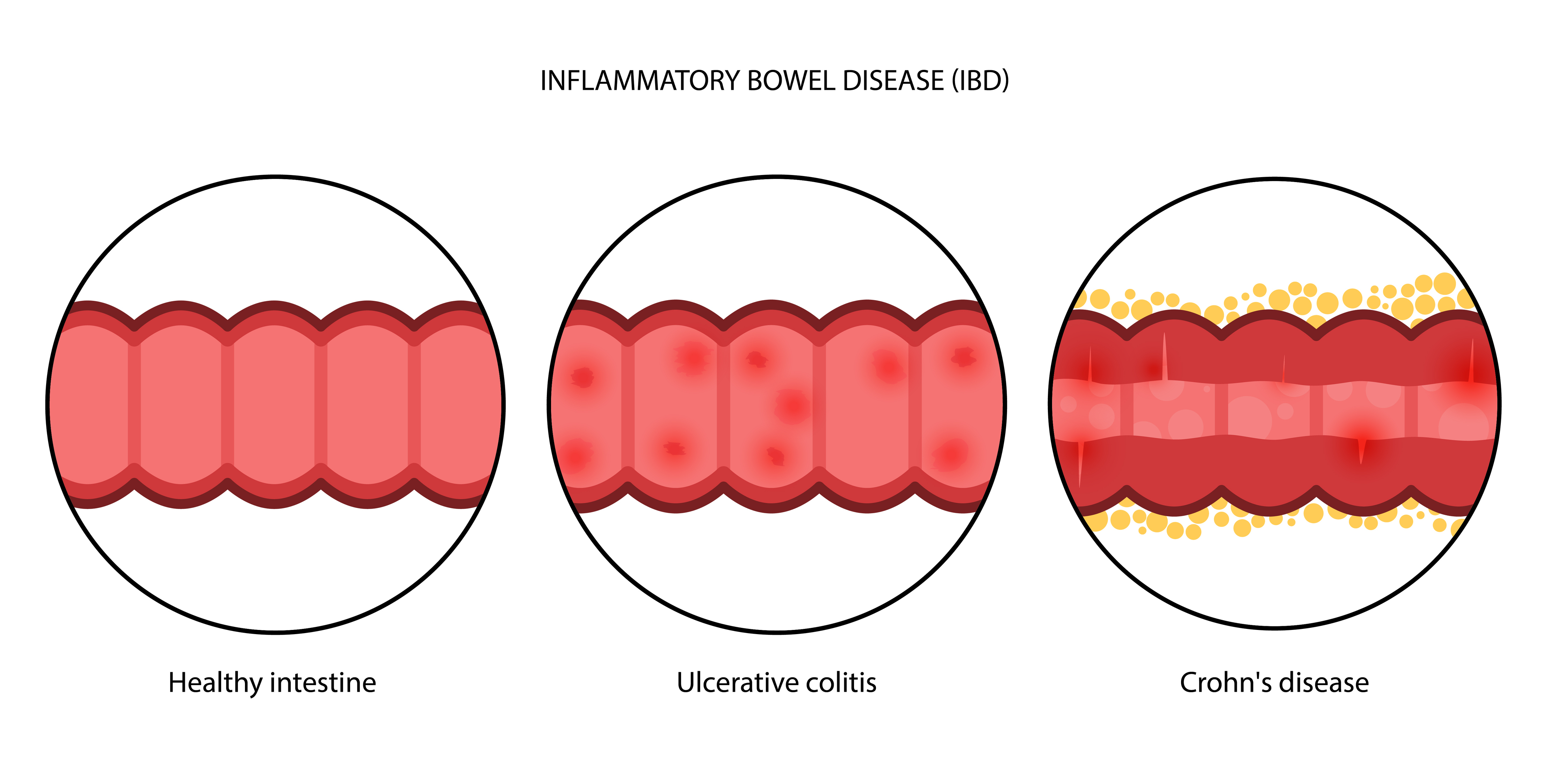
Crohn's disease can manifest in a variety of symptoms, which can vary widely in severity and frequency. Common symptoms include persistent diarrhea, abdominal pain, and cramping, which often occur in the lower right part of the abdomen. Individuals may also experience fatigue, weight loss, and malnutrition due to poor absorption of nutrients. Rectal bleeding and a sense of urgency to defecate are also indicative of the disease. In severe cases, symptoms can lead to complications such as bowel obstruction, fistulas, and ulcers.
Early recognition of these symptoms is critical for timely diagnosis and treatment. Chronic inflammation can lead to scarring and narrowing of the intestines, exacerbating symptoms and leading to additional health issues. Regular monitoring and communication with healthcare professionals are essential for managing symptoms effectively.
Diagnosing Crohn's disease involves a combination of medical history, physical examination, and diagnostic tests. Blood tests are often performed to check for signs of inflammation and anemia. Stool tests can help rule out infections and detect the presence of blood. Imaging studies, such as CT scans and MRIs, provide detailed pictures of the intestines, revealing areas of inflammation and other abnormalities.
Endoscopic procedures, including colonoscopy and sigmoidoscopy, are critical for visualizing the interior of the colon and terminal ileum. During these procedures, biopsies may be taken to examine tissue samples for characteristic changes associated with Crohn's disease. Capsule endoscopy, which involves swallowing a small camera that captures images of the entire digestive tract, is another valuable diagnostic tool.
Treatment for Crohn's disease aims to reduce inflammation, manage symptoms, and achieve and maintain remission. Medications play a central role in managing the disease. Aminosalicylates (5-ASAs) are often used to control mild to moderate inflammation, while corticosteroids are prescribed for more severe flare-ups to quickly reduce inflammation. Immunomodulators and biologic therapies are used for long-term management, targeting the immune system to prevent inflammation.
Biologic therapies, such as anti-TNF agents, have revolutionized the treatment of Crohn's disease. These medications target specific proteins involved in the inflammatory process, offering significant relief for many patients. However, they require careful monitoring for potential side effects, including infections.
In some cases, surgery may be necessary to address complications like strictures, fistulas, or abscesses. Surgical interventions aim to remove damaged sections of the intestine and restore normal function. Post-surgical care and ongoing medical treatment are crucial for preventing recurrence.
Nutrition plays a pivotal role in managing Crohn's disease. A balanced diet tailored to individual needs can help alleviate symptoms and prevent malnutrition. Patients are often advised to avoid foods that trigger symptoms, such as high-fiber foods, dairy products, and fatty or fried foods. Small, frequent meals and adequate hydration are also recommended.
Nutritional supplements, including vitamins and minerals, may be necessary to address deficiencies caused by malabsorption. Working with a dietitian can help patients develop a personalized nutrition plan that supports their health and well-being.
Lifestyle changes, such as regular exercise, stress management, and quitting smoking, can also improve symptoms and overall quality of life. Exercise promotes digestive health and reduces stress, which can exacerbate symptoms. Mindfulness practices, yoga, and other stress-reducing activities can help manage the psychological impact of living with a chronic illness.
Living with Crohn's disease can be challenging, both physically and emotionally. Psychological support, including counseling and support groups, is essential for coping with the chronic nature of the disease. Mental health professionals can provide strategies for managing stress, anxiety, and depression, which are common among individuals with Crohn's disease.
Support groups offer a sense of community and shared experience, helping patients feel less isolated. Connecting with others who understand the challenges of living with Crohn's disease can provide valuable emotional support and practical advice.
Ongoing research continues to enhance our understanding of Crohn's disease and improve treatment options. Advances in genetics, microbiome studies, and immunology are uncovering new insights into the underlying causes of the disease. Clinical trials are testing novel therapies that aim to provide more effective and personalized treatment options.
Emerging treatments, such as stem cell therapy and advanced biologics, hold promise for better managing the disease and improving patients' quality of life. Staying informed about the latest research developments and participating in clinical trials can provide access to cutting-edge treatments and contribute to the advancement of medical knowledge.
Understanding Crohn's disease, recognizing its symptoms, and exploring comprehensive treatment approaches are crucial for managing this chronic condition effectively. With early diagnosis, personalized treatment plans, and ongoing support, individuals with Crohn's disease can lead fulfilling lives. Continuous advancements in medical research offer hope for even better management and potential cures in the future.