According to statistics from the United States, urinary incontinence affects millions of adults, with a higher prevalence in women than in men. With the advent of an aging society, the incidence of urinary incontinence has been increasing year by year and has become an important public health issue.
 1. Early identification: understanding the symptoms of urinary incontinence
1. Early identification: understanding the symptoms of urinary incontinenceEarly identification of urinary incontinence is essential for timely intervention and treatment. Many patients may ignore the symptoms of urinary incontinence due to shame or lack of understanding of the nature of the disease, leading to worsening of the condition. The U.S. Guidelines for the Prevention and Treatment of Urinary Incontinence emphasize that early identification of signs of urinary incontinence and taking appropriate measures can effectively relieve symptoms and improve treatment outcomes.
Common symptoms:
Urgent urinary incontinence (Overactive Bladder, OAB): Patients often feel a strong urge to urinate without warning and have difficulty controlling urination. Urgent urinary incontinence is often accompanied by frequent urination (more than eight times a day) and may lead to nocturnal incontinence.
Stress Incontinence: This type of incontinence occurs when there is increased abdominal pressure, such as when coughing, sneezing, laughing, lifting heavy objects or exercising. It is usually due to relaxation of the pelvic floor muscles or malfunction of the urethral sphincter.
Mixed Incontinence: This type is a combination of urge incontinence and stress incontinence. Patients will experience incontinence symptoms in both cases.
Overflow Incontinence: This type of incontinence usually occurs when the bladder cannot be completely emptied, resulting in urine overflow. Its symptoms include frequent urination, nocturia, weak urine flow, etc.
Key points for early identification:
Pay attention to symptoms such as frequent urination, urgency, difficulty urinating or involuntary leakage of urine.
Pay attention to changes in quality of life, especially the impact on activities, social and psychological status.
Encourage patients to be open and discuss these symptoms with their doctors, and avoid viewing urinary incontinence as a "normal" or "inevitable" part of the aging process.
By identifying and recording these symptoms in a timely manner, patients and doctors can take intervention measures earlier to prevent further development of urinary incontinence.
There are many types and causes of urinary incontinence, and understanding these common types can help patients and medical staff develop more appropriate treatment plans. According to the American Guidelines for the Prevention and Treatment of Urinary Incontinence, urinary incontinence is mainly divided into the following types:
1) Stress Incontinence
Cause: Stress urinary incontinence is usually associated with weakening of the pelvic floor muscles or urethral sphincter. The pelvic floor muscles play a vital role in supporting organs such as the bladder, uterus, and rectum. Factors such as childbirth, obesity, and aging can all lead to weakening of the pelvic floor muscles, which in turn cause urinary incontinence.
Characteristics: Urine flows out involuntarily during urination, especially when coughing, sneezing, laughing, exercising, etc. increase abdominal pressure.
2) Urgency Incontinence
Cause: Urgency incontinence is mostly caused by overactive bladder (OAB). The bladder smooth muscle contracts abnormally, and the patient feels a strong urge to urinate and has difficulty controlling it, resulting in urine leakage. Age, neurological problems (such as stroke or Parkinson's disease), and diabetes are common predisposing factors.
Characteristics: Patients usually experience frequent urges to urinate and sudden incontinence, especially at night or in stressful situations.
3) Mixed Incontinence
Cause: Mixed incontinence is a combination of stress incontinence and urge incontinence. Patients may experience alternating symptoms of these two types.
Characteristics: Often accompanied by two types of symptoms, patients may leak urine when coughing or exercising, or may be unable to control the sudden urge to urinate.
4) Overflow Incontinence
Cause: Overflow incontinence is usually caused by the inability to completely empty the bladder, which may be related to urethral obstruction (such as prostatic hyperplasia) or nerve damage (such as spinal cord injury, diabetic neuropathy).
Characteristics: The bladder is overfilled for a long time, and eventually overflows.
Understanding the types and causes of urinary incontinence can help patients communicate better with doctors and help develop personalized treatment plans.
Accurate diagnosis is the prerequisite for urinary incontinence treatment. The American Guidelines for the Prevention and Treatment of Urinary Incontinence recommend a series of comprehensive diagnostic steps to ensure that doctors can fully understand the patient's condition.
1) History collection and symptom assessment
Doctors usually ask patients in detail about their symptoms, including the frequency, situation, and accompanying symptoms of urinary leakage.
Symptom questionnaires (such as the International Urinary Control Questionnaire, ICIQ) and urination diaries help assess the severity of symptoms.
2) Physical examination
Physical examination includes examination of the abdomen, pelvis, rectum and urethra to assess whether there are anatomical abnormalities or pelvic floor muscle dysfunction.
3) Urodynamic examination
Urodynamic examination is the gold standard for evaluating bladder and urethral function, and is mainly used to diagnose conditions such as overactive bladder and urethral obstruction. By measuring data such as bladder pressure during filling, urination and post-urination, urine flow, etc., doctors can better understand the cause of urinary incontinence.
4) Imaging examination
Ultrasound examination can be used to evaluate bladder capacity, residual urine volume and urethral anatomy.
For some patients, CT or MRI may be required to evaluate anatomical problems of the urinary system.
Through these diagnostic methods, doctors can accurately determine the type of urinary incontinence and its cause, thereby providing a basis for formulating treatment plans.
There are many treatment methods for urinary incontinence, and the treatment strategies vary according to the different types of urinary incontinence. The American Guidelines for the Prevention and Treatment of Urinary Incontinence provide treatment recommendations for different types of urinary incontinence.
1) Behavioral therapy
Bladder training: Improve bladder control by timing and delaying urination.
Pelvic floor muscle training (PFMT): Kegel exercises, which can enhance the strength and endurance of pelvic floor muscles and help treat stress urinary incontinence.
Lifestyle intervention: Including reducing caffeine and alcohol intake, controlling weight, etc.
2) Drug treatment
Anticholinergic drugs: Used to treat overactive bladder and urge incontinence, can reduce involuntary bladder contractions.
Alpha-receptor agonists: Commonly used to treat urinary incontinence caused by prostatic hyperplasia in men.
Local estrogen therapy: Especially suitable for women, it can improve the health of pelvic floor tissues and relieve urinary incontinence symptoms.
3) Surgical treatment
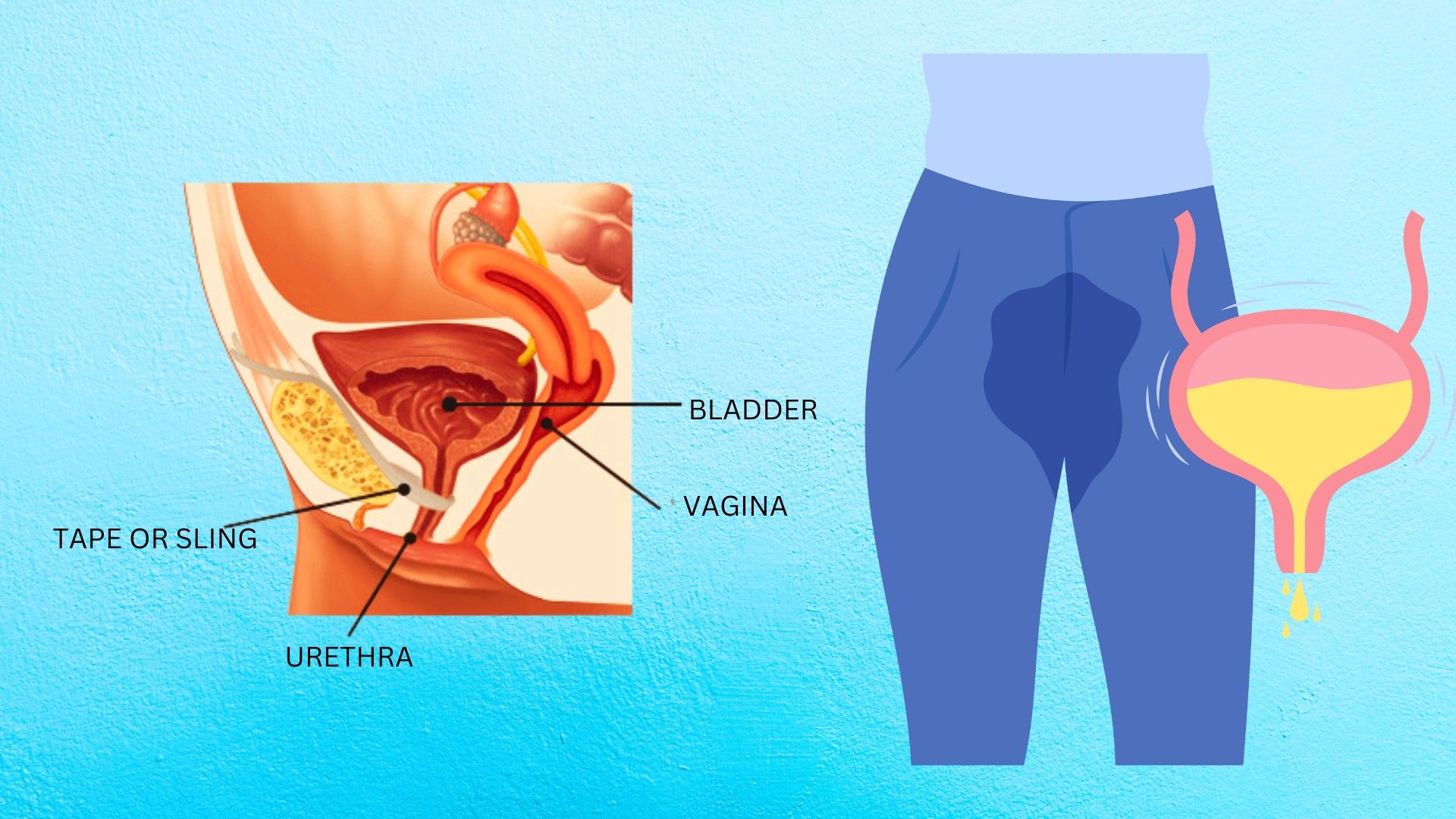
Sling procedure: Mainly used to treat stress urinary incontinence, by implanting a belt or mesh to support the urethra.
Bladder stimulation therapy: Regulate bladder function by electrically stimulating the bladder, suitable for patients with overactive bladder.
Artificial urinary sphincter: Suitable for men with severe urinary incontinence, usually caused by prostate removal and other reasons.
4) Other therapies
Local treatment: Such as local drug therapy, physical therapy, etc., to improve symptoms.
Assistive devices:
Such as urinary incontinence pads, urinary catheters, etc., for convenient treatment in daily life.
Prevention of urinary incontinence should start with lifestyle changes. The American Guidelines for the Prevention and Treatment of Urinary Incontinence provide some effective preventive measures to help patients reduce the risk of urinary incontinence.
Maintain a healthy weight: Obesity is one of the main risk factors for urinary incontinence. Maintaining a healthy weight through diet control and regular exercise can significantly reduce the incidence of urinary incontinence.
Avoid excessive burden on the pelvic floor: Avoid long-term excessive force (such as forceful defecation when constipated), and perform appropriate pelvic floor muscle exercises to strengthen the pelvic floor muscles.
Avoid drug abuse: Certain drugs (such as diuretics, sedatives) may aggravate the symptoms of urinary incontinence. Patients should use drugs under the guidance of doctors.
Regular urination training: Regular urination can avoid overfilling of the bladder and reduce the risk of urinary incontinence.
Urinary incontinence is not only a physiological problem, it also involves the patient's psychological, social life and overall quality of life. The key to long-term management of urinary incontinence lies in the patient's active cooperation and the continuous implementation of the treatment plan.
Psychological support: Many patients with urinary incontinence will face emotional problems, such as anxiety and depression. Providing psychological support, education and social support can help patients maintain a positive attitude and improve treatment compliance.
Social adaptation: Encourage patients to participate in social activities and avoid isolation. Through education and support, patients can better adapt to changes in life and improve their quality of life.
The prevention and treatment of urinary incontinence is a complex and multifaceted process involving early identification, accurate diagnosis, scientific treatment and long-term management. The U.S. Guidelines for the Prevention and Treatment of Urinary Incontinence provide a scientific basis for patients and medical professionals to help patients improve symptoms and improve their quality of life through timely intervention and comprehensive treatment. The occurrence of urinary incontinence and its negative impact on life can be effectively reduced by maintaining a healthy lifestyle, engaging in appropriate exercise and weight management, and seeking professional treatment when symptoms occur.